Listeria and You
Lately you may have seen news headlines about Listeria (or Listeria monocytogenes) outbreaks and food recalls — frozen pasta meals, cut fruit, deli meats, etc. One might wonder: is this just media alarmism, or should you as patients in Colorado really be concerned?
At Homestead Direct Primary Care, we believe informed patients make safer choices. Below is a helpful write-up to explain:
What Listeria is and why it’s getting attention
Who’s at higher risk
How this applies here in Colorado
Practical prevention tips
When to call us (or a medical provider)
What is Listeria, and why is it in the news?
Listeria monocytogenes is a bacteria capable of causing listeriosis, a serious foodborne infection. CDC+3CDC+3CDC+3
Some key facts:
It can survive and even grow at refrigeration temperatures (in contrast to many bacteria), which makes it trickier to control. U.S. Food and Drug Administration+3Mayo Clinic+3U.S. Food and Drug Administration+3
In the U.S., around 1,600 infections and ~260 deaths occur annually (though many cases may go unreported) CDC+2CDC+2
In recent days, a multistate outbreak linked to ready-to-eat pasta meals sold by Walmart, Trader Joe’s and others has been publicized. The implicated products have been recalled or pulled from shelves. 9News+4Health+4San Francisco Chronicle+4
Also, fresh-cut fruit (cantaloupe) products recently underwent recall due to possible Listeria contamination. Allrecipes
These outbreaks get attention because:
The illness can be severe (hospitalization, even death) in vulnerable groups.
The food items are widely distributed, often ready-to-eat (so no cooking step to kill bacteria).
They highlight gaps in food safety surveillance, processing, and handling.
So the “hype” is not purely sensational — it reflects real risk, especially in certain populations.
Who is most at risk?
While many healthy adults may eat a contaminated food without serious consequence, certain groups are at significantly higher risk of invasive disease (where the bacteria spread beyond the gut):
Pregnant people / fetuses / newborns — Listeria can cross the placenta and lead to miscarriage, stillbirth, premature birth, or severe neonatal infection. CDC+4CDC+4PMC+4
Older adults (especially over 65) CDC+2CDC+2
People with weakened immune systems — e.g. on immunosuppressants, chemotherapy, HIV, chronic illnesses like liver/kidney disease, or after transplantation. CDC+2NCBI+2
People using acid suppression medications (like PPIs) may have higher susceptibility because stomach acid is less able to kill the bacteria. NCBI
For those in these risk categories, getting listeriosis is more likely to lead to a serious infection (e.g. bloodstream infection, meningitis) rather than just mild gastrointestinal symptoms. CDC+2CDC+2
Why Colorado patients should pay attention
Colorado has had past Listeria outbreaks. The infamous 2011 U.S. listeriosis outbreak was traced to cantaloupes grown in Colorado (Jensen Farms), leading to dozens of deaths. Wikipedia+2Marler Clark+2
Most recently, national recalls of ready-to-eat food items (pasta meals) and cut fruit products affect distribution chains that may reach Colorado grocery stores. U.S. Food and Drug Administration+5Health+59News+5
Colorado’s citizens and supply chains are not isolated; product recalls are national and may reach our state.
Although reports do not currently (to my knowledge) show a localized Colorado spike, this is precisely the time to re-emphasize prevention.
Thus, it’s prudent for our patient population — especially the higher-risk groups — to be aware and act with caution.
What patients can do: practical prevention advice
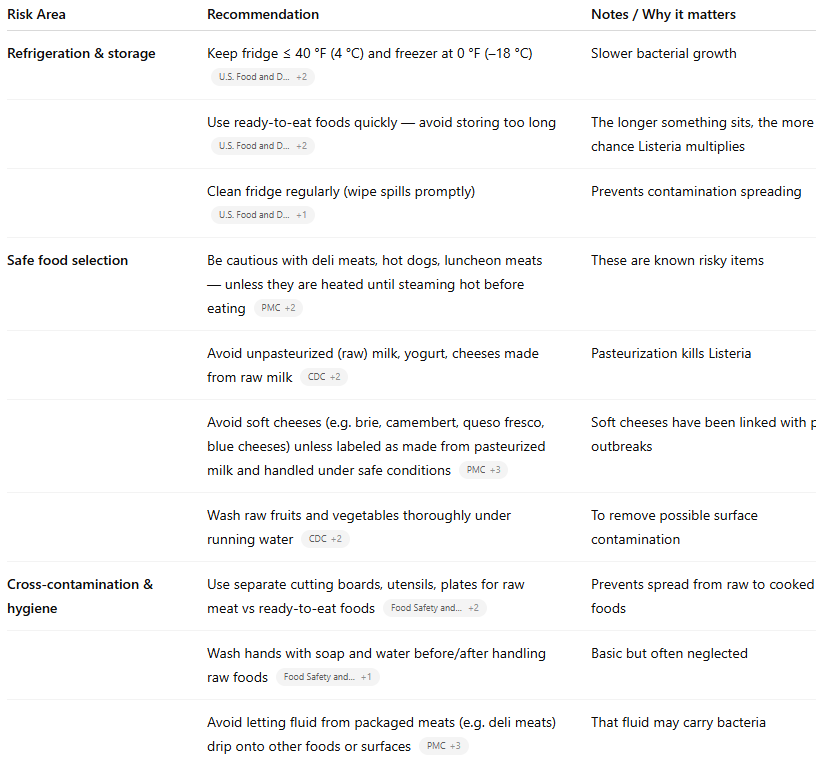
Fortunately, many of the risks can be mitigated with careful food handling. Below are evidence-based practices recommended by CDC, FDA, USDA, and clinical sources. CDC+8CDC+8U.S. Food and Drug Administration+8
Note: If a food product recalls or safety alert involves your area, don’t wait for symptoms to act — discard the product and sanitize spaces where it touched.
When to seek medical care or contact Homestead DPC
While most healthy adults with mild symptoms do not require special treatment, some situations warrant medical evaluation. Mayo Clinic+3CDC+3CDC+3
Be alert for symptoms, especially in high-risk people
Symptoms of invasive listeriosis may appear within weeks (commonly within 2 weeks) after ingestion, though onset can vary. CDC+2CDC+2
Typical symptoms:
Fever, chills, muscle aches
Fatigue, general malaise
Gastrointestinal symptoms (nausea, diarrhea, vomiting)
In more serious cases: headache, stiff neck, confusion, loss of balance, seizures CDC+2CDC+2
In pregnancy: symptoms may be mild (flu-like), but risks to fetus are high CDC+2ACOG+2
What to do if you have symptoms + relevant exposure
If you’ve eaten a recalled food, or suspect exposure (e.g. deli meats, soft cheeses, recall item) and develop fever or symptoms above, you should contact your healthcare provider. Let them know:
What you ate and when
If you are pregnant or immunocompromised
For high-risk persons (pregnancy, immunocompromised, older adults) with symptoms + exposure, clinicians often consider testing and empiric treatment (blood cultures, possibly CSF testing, antibiotics like IV ampicillin + gentamicin) depending on the severity. CDC+2CDC+2
If the blood culture grows Listeria, the standard therapy is IV ampicillin plus gentamicin for 14–21 days (or adjusted in allergic patients) depending on the site of infection. CDC+1
For asymptomatic people who merely ate a recalled product (without symptoms), most experts do not recommend antibiotics or testing — but emphasize monitoring and prompt evaluation if symptoms arise. CDC+1
At Homestead DPC, we are ready to consult with you, order appropriate tests, and guide management if there is concern for Listeria exposure or early symptoms.
Final thoughts & recommendations for Homestead DPC patients
The current media attention on Listeria is real and underlines existing vulnerabilities in our food supply.
For most healthy patients, the risk remains low — but for those in high-risk groups (pregnant, older, immunocompromised), vigilance is wise.
The good news: many preventive steps are simple and already part of safe food practices (proper refrigeration, cooking, avoiding risky foods, avoiding unpasteurized products).
Stay alert to recalls and food safety alerts.
Don’t hesitate to contact us if you believe you’ve had exposure, especially if symptoms develop.